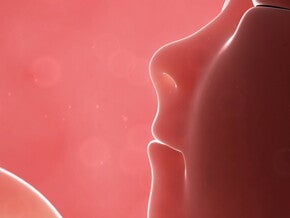
This is called the vertex presentation.
A small percentage of babies lie in a transverse or shoulder presentation, which may result in a Caesarean delivery.
A breech presentation occurs when the baby’s bottom moves into the pelvis and occurs in 3–4% of cases. It may be possible to turn the baby manually by external cephalic version after 37 weeks, or even in early labour. A vaginal birth may be allowed if all the clinical features of a persistent breech presentation are favourable. If not, a Caesarean section is usually recommended, as it poses less risk to mother
and baby.
Foetal positions
The position of the baby refers to the relationship of the presenting part to the mother’s pelvis. The most common is the anterior position in which the back of the baby’s head is toward the mother’s abdomen.
The posterior position, when the back of the baby’s head is against the mother’s spine, often results in prolonged labour and a great deal of back discomfort.
Precipitate labour
Precipitate labour is a quick labour, usually shorter than three hours. Contractions are intense and there is no time to adapt slowly to labour. You will need to use all the pain management skills you have at your disposal.
Prolonged labour
Prolonged labour is a labour which lasts more than 24 hours, and is usually caused by one or a combination of the following:
- Ineffective contractions.
- High presenting part-posterior position.
- Large baby.
- Small pelvis.
- Extreme tension.
- Large amount of medication.
- Induction of labour.
The baby will be closely monitored during prolonged labour. You will need patience and encouragement. You may want to consider alternative options, for example an epidural for pain relief.
Back labour
Back labour is usually caused by a posterior position, a breech presentation, or labouring on your back. The extreme discomfort can be relieved by:
- Applying heat.
- Counter-pressure and massage.
- Changing positions, to take pressure off your back.
- Pelvic rocking on all fours.
- Lying on your side.
To learn more about the different positions in labour, click here.
Counter-pressure and massage can be soothing if you have a back labour.
Interventions
Various procedures can be used during labour to provide diagnostic information, prevent possible complications, and even alter the course of your labour. Discuss these with your caregiver before labour and become familiar with them all.
Intravenous fluids
Some doctors use intravenous fluids (IVs or drips) routinely and others only when indicated. The IV is administered through a needle into the vein. It is used to prevent dehydration and administer drugs and medication. It is used with inductions, epidurals and general anaesthesia. It may limit your mobility; if so, request a stand on wheels to support you while you walk around.
A catheter, rather than a drip, may be placed in an arm vein with a side-port for painkilling or other injections. A drip can be connected to it as needed.
Electronic foetal monitor
The electronic monitor measures the intensity and duration of the uterine contractions, as well as the baby’s heart rate. The external monitor consists of two belts placed around your abdomen, one to measure the foetal heart rate and the other to measure the strength of contractions. The monitor assesses the wellbeing of your baby in case complications arise.
Induction
An induced labour is one which is started either chemically or with physical stimulation. The contractions may be stronger, longer and more difficult than during natural labour. Encouragement and support are essential.
Medical reasons for inducing labour:
- When a complication arises such as hypertension, pre-eclampsia, heart disease, gestational diabetes, or bleeding during pregnancy.
- Baby is in danger of not getting enough nutrients/oxygen from placenta.
- Amniotic sac has ruptured but labour hasn’t started within 24–48 hours.
- Pregnancy is prolonged beyond 42 weeks.
- Infection develops inside uterus known as chorioamnionitis.
Indications for an induction
- Continuation of the pregnancy could adversely affect either the mother or the baby.
- Prolonged rupture of membranes with no labour starting. Hypertension or pre-eclampsia.
- Post-maturity.
Techniques
- Inserting a pessary (any of various devices worn in the vagina to support or correct the position of the uterus or rectum) containing prostaglandin into the vagina.
- Artificially rupturing the membranes by inserting a plastic amnion hook through the vagina and making a small tear in the membranes. In women who are, or may be, HIV-positive, it is better to avoid rupturing the membranes.
- Administering syntocinon, a synthetic form of the hormone oxytocin, to induce or speed up labour. It is usually administered intravenously but is also available in tablet form, placed under the tongue and absorbed through the mucous membranes.
Episiotomy
This is a surgical incision into the perineum to enlarge the vaginal opening. The need for an episiotomy is usually determined when the baby’s head begins to stretch the perineum. You may not feel the incision due to a natural numbness caused by the stretching. You will need a local anaesthetic to repair the episiotomy after delivery.
Advantages
- Enlarges the vaginal opening.
- May hasten delivery of the baby.
- Gives more space if vacuum extractor or forceps are used.
- Reduces pressure on the head of a premature baby.
Disadvantages
- Causes pain and discomfort after birth.
- May affect intercourse for several months.
- Incision area may bleed excessively or become infected.
Forceps
Forceps are stainless steel instruments which can be inserted into the vagina and placed on either side of the baby’s head. They are used to assist the delivery of the baby’s head.
Forceps Detail
Advantages
- Speeds up delivery, if necessary.
- Assists the delivery of the baby when anaesthesia is used, or your ability to
push is reduced. - Helps protect the premature baby’s head from prolonged pressure.
- Assists the birth of the head with a breech vaginal birth.
- Helps turn the baby’s head to an anterior position.
Disadvantages
- Usually needs an episiotomy.
- May bruise soft tissues of the baby’s head or face.
- Increases the need for regional anaesthesia.
- May traumatise the mother’s vaginal tissues.
Vacuum extractor
Vacuum Detail
This cup-like device is applied to the baby’s head. It may be made of metal or flexible plastic. A rubber tube extends from the cap to a vacuum pump that creates suction. The doctor, pulling on the cap during contractions, helps the baby move down the birth canal.
Advantages
- Helps descent, requiring less vaginal space than forceps.
- Can be applied to the baby at a higher position in the pelvis than forceps.
Disadvantages
- May cause bruising or swelling of the soft scalp tissue of the baby.
- Is not as effective as forceps in turning the baby’s head.
CHECKLIST – BIRTH PLAN
Also make checklist available in the mommy’s tool tab. Ensure all checklists are designed as a tool. Should be in a format that can be printed out by mom.
- Pubic shaving.
- Enemas.
- IVs/Drips.
- Foetal monitoring.
- Labour positions – active versus passive.
- Inductions.
- Episiotomy versus tearing.
- Forceps, vacuum extractor.
- Type of anaesthesia – epidural, spinal, general.
- Partner’s presence.
- Holding your baby immediately after birth.
- Baby to breast and chest in operating theatre while mother’s wound is
closed.
For more information on a vaginal birth, consult the following sources:
- Caregiver.
- Childbirth educator.
- Childbirth associations.